Background: State medical cannabis laws may lead patients with chronic noncancer pain to substitute cannabis in place of
prescription opioid or clinical guideline-concordant nonopioid prescription pain medications or procedures.
Objective: To assess the effects of state medical cannabis laws on the receipt of prescription opioids, nonopioid prescription pain
medications, and procedures for chronic noncancer pain.
Design: Using data from 12 states that implemented medical
cannabis laws and 17 comparison states, augmented synthetic control analyses estimated laws’ effects on the receipt of chronic
noncancer pain treatment, relative to predicted treatment receipt in the absence of the law.
Setting: United States, 2010 to 2022.
Participants: 583 820 commercially insured adults with chronic noncancer pain.
Measurements: Proportion of patients receiving any opioid prescription, nonopioid prescription pain medication, or procedure for chronic noncancer pain; the volume of each treatment type; and mean days’ supply and mean morphine milligram equivalents per day of prescribed opioids, per patient in a given month.
Results: In a given month during the first 3 years of law implementation, medical cannabis laws led to an average difference of 0.05 percentage points (95% CI, 0.12 to 0.21percentage points), 0.05 percentage points (CI, 0.13 to 0.23 percentage points), and 0.17 percentage points (CI, 0.42 to 0.08 percentage points) in the proportion of patients receiving any opioid prescription, any nonopioid prescription pain medication, or any chronic pain procedure, respectively, relative to what we predict would have happened in that month had the law not been implemented.
Limitations: This study used a strong nonexperimental design but relies on untestable assumptions involving parallel counterfactual trends. Statistical power is limited by the finite number of states. Results may not generalize to noncommercially insured populations.
Conclusion: This study did not identify the important effects of medical cannabis laws on the receipt of opioid or nonopioid pain treatment among patients with chronic noncancer pain.
Primary Funding Source: National Institute on Drug Abuse. Ann Intern Med. doi:10.7326/M23-0053 Annals.org For author, article, and disclosure information, see the end of the text. This article was published at Annals.org on 4 July 2023.
In 2019, 21% of U.S. adults experienced chronic noncancer pain, defined as pain from conditions other than cancer that occurs on at least half of the day for 3 or more months (1). In the 38 states and the District of Columbia (D.C.) with medical cannabis laws, people with chronic noncancer pain are eligible to use cannabis for pain management (2). The cannabis industry and advocates have asserted that state medical cannabis laws offer a partial solution to the opioid overdose crisis in the United States, which took more than 80 000 lives in 2021 (3), via substitution of cannabis in place of prescription opioids for chronic noncancer pain (4–7). Although clinical guidelines have emphasized prescription opioids as the first-line treatment of chronic non-cancer pain management (8–11), guidelines do not recommend cannabis. Instead, current clinical guidelines emphasize nonopioid, non-cannabis treatments including medications (for example, anticonvulsants) and procedures (for example, physical therapy) (11). Evidence on the effectiveness of cannabis for chronic noncancer pain is limited, mixed, and subject to varying interpretations. Rigorous evidence reviews covering largely identical bodies of research have come to disparate conclusions about the effectiveness and whether the risks of cannabis use for chronic noncancer pain—including addiction and potential adverse mental health side effects—outweigh the benefits (12, 13). Prior studies have suggested an association between
state medical cannabis laws and reduced prescription opioid use, interpreting this finding as being driven by the substitution of cannabis in place of opioids for chronic noncancer pain (14–21). However, this research is limited by the general population and repeated cross-sectional samples in which most people do not have chronic noncancer pain, and changes in pain treatment within persons over time are not observed. People who use medical cannabis are more likely than their counterparts to use and misuse prescription opioids (22, 23), and a prospective study found no association between cannabis use among people with chronic non-cancer pain and future prescription opioid use (24). To our knowledge, no prior studies have examined how state medical cannabis laws influence the receipt of guideline-concordant nonopioid, non-cannabis pain treatments among patients with chronic noncancer pain. Our study assesses the effects of medical cannabis laws on patterns of prescription opioid and clinical guideline–concordant nonopioid treatments for chronic noncancer pain among commercially insured U.S. adults.
METHODS: This manuscript follows the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for observational studies (Section A of the Supplement, available at Annals.org).
Design: The study design follows the target trial emulation framework (Appendix Table 1, available at Annals.org) for strengthening nonexperimental studies by “emulating” a hypothetical randomized trial. We identified 12 states that implemented medical cannabis laws and did not have laws in place legalizing the recreational use of cannabis between 2014 and 2019 (Arkansas, Connecticut, Florida, Louisiana, Maryland, Minnesota, North Dakota, New Hampshire, New York, Oklahoma, Ohio, and Pennsylvania). Each medical cannabis law state had a unique 7-year analytic study period including 4 years of prelaw data and 3 years of postlaw data. The earliest state-specific study period began in September 2010, and the latest state-specific study period ended in July 2022 (Appendix Table 2, available at Annals.org). Using data from 17 comparisons states that did not have medical cannabis laws between 2010 and 2022 (Alaska, Georgia, Idaho, Indiana, Iowa, Kansas,
Kentucky, Mississippi, Nebraska, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Virginia, Wisconsin, and Wyoming), we constructed 12 unique comparison groups aligned with each medical cannabis law state’s specific 7-year study period.
Data: We used OptumLabs Data Warehouse unidentified administrative insurance claims from September 2010 to July 2022, which include medical and pharmacy claims for services covered by commercial and Medicare Advantage insurance plans for 30 million adults aged 18 years and older per year. We used state medical cannabis law data compiled by 2 public health attorneys (A.D.M. and L.R.). These data were assembled using standard legal epidemiology techniques, including systematic searches of statutes and regulations in the Westlaw data-
base and identification of state session laws and regulatory materials (25, 26). Our legal research confirmed that chronic noncancer pain was a qualifying condition for all 12 medical cannabis laws included in this study.
Sample: In each of the 12 medical cannabis law states, we created an analytic sample of adults aged 18 years or older who were continuously enrolled in commercial or Medicare Advantage insurance for that state’s 7-year study period and were diagnosed with conditions that
commonly lead to chronic noncancer pain (arthritis, low back pain, serious headache, fibromyalgia, neuropathic pain) (27). Patients were included if they had 1 inpatient or 2 outpatient diagnosis codes for a given condition in the 4 years before the medical cannabis law implementation. Patients meeting this criterion for more than 1 chronic noncancer pain condition were coded as having each
condition (see Appendix Table 3, available at Annals.org, for diagnosis codes). We then created 12 distinct comparison groups, 1 for each medical cannabis law state, that included adults from the 17 comparison states who were continuously enrolled in commercial or Medicare Advantage insurance for the relevant 7-year study period and met chronic non-cancer pain diagnostic criteria in the first 4 years of that period.
Measures: Chronic noncancer pain treatment outcome measures were constructed at the patient-month level and then aggregated to the state-month level for primary analyses. Aggregate state data are appropriate given the study’s focus on estimating the effects of medical cannabis laws on chronic pain treatment at the state population, as opposed to individual patient, level. Month-level data capture clinically meaningful chronic noncancer pain treatment outcomes as guidelines recommend frequent treatment of many patients, and prescriptions are commonly administered on a monthly basis. In addition, analysis at the monthly level captures granular trends in outcomes over the prelaw period; as noted in Statistical Analysis below, accurately capturing prelaw trends is a key component of our analytic approach. We conducted a secondary analysis using state-year-level measures. Prescription opioid measures included the proportion of patients who received any opioid prescription; the mean number of opioid prescriptions per patient pre-scribed opioids; mean days’ supply and mean morphine milligram equivalents (MMEs) per day per patient prescribed opioids; and the proportion of patients prescribed opioids who received any opioid prescription with greater than 7 days’ supply or greater than 50 MMEs per day across all opioid prescriptions—indicators of high-risk prescriptions that increase risk for overdose (10, 11)—accounting for overlapping prescriptions, per state per month. Opioid pain medications were identified using the Centers for Disease Control and Prevention (CDC) Opioid National Drug Code (NDC) and Oral MME Conversion File. Opioid agonist medications used primarily to treat opioid use disorder were excluded (Appendix Table 3). We also measured the proportion of patients receiving any clinical guideline–concordant prescription nonopioid pain medication or procedure per state per month and the mean number of medications or procedures among patients receiving these treatments, per state per month. The chronic pain physician author (M.C.B.) reviewed clinical guidelines to determine these treatments and developed algorithms to identify them in claims data (Appendix Table 3). State laws were coded as binary indicators that changed from 0 to 1 in the first month that a state law was implemented for 15 or more days. Following prior literature, we defined each state’s medical cannabis law implementation date as the day the state’s first medical cannabis dispensary opened for business; of the 12 medical can-nabis law states, only 1 (Oklahoma) had provisions allowing patients to grow cannabis at home, meaning that—in most states—patients could not legally access cannabis for medical use until dispensaries opened (28–30). Covariates were measured at the state-year level and included the proportion of patients who were female; the mean patient age; the mean patient Elixhauser Comorbidity Index; the proportion of patients with a mental illness diagnosis; and the proportion of patients with a substance use disorder diagnosis per state per year.
Statistical Analysis: We used an augmented synthetic control approach (31), which weights comparison states so that the outcomes during the prelaw period are identical in the intervention and comparison states. This method creates a weighted comparison group—a “synthetic control”—that estimates what would have happened to the outcome of interest in the state implementing a new law in the absence of that law. In the augmented synthetic control approach, the estimated effect of the law can be thought of as the difference in differences in outcomes before and after the law in the state implementing the law and its synthetic control. Because the augmented synthetic control approach equalizes the prelaw measures between the state implementing the law and its synthetic control, the law’s effect on an outcome at a given post-law time point is equal to the difference in that outcome between the state implementing the law and its synthetic control at that time. The key assumptions underlying the augmented synthetic control approach are that there are sufficient prelaw time periods to estimate what would have happened to the trajectory of the outcome of interest in the treatment state in the absence of the law; that absent the law, trends in outcomes in the treatment state would have followed the same path as trends in outcomes in the synthetic control; that 1 state’s law does not influence outcomes in other states; and that there is no “anticipation effect” in which out-comes change, before law implementation, in anticipation of the pending law. These assumptions are described in more detail in Appendix Table 1. Using the augmented synthetic
control approach, our study sought to answer the question: among states that implemented a medical cannabis law, what was the effect of the law on outcomes relative to what would have been observed had those states not implemented a medical cannabis law? Using the augmented synthetic control approach, for each of the 12 states that implemented a medical cannabis law, we constructed the synthetic control as the weighted average of comparison states best approximating chronic noncancer pain treatment outcomes and covariates in the
age of the state-specific estimates (32). We estimated the difference in outcomes attributable to medical cannabis laws averaged over the entire 3-year post-law period as well as month-by-month changes in outcomes attributable to the laws, which capture flexible differences in outcome trajectories due to implementation ramp-up or other factors. Secondary analyses were conducted at the state-year level. We conducted a sensitivity analysis controlling for state laws that limited the dose and/or duration of opioid prescribing (33) during the study period. Confidence intervals indicate that the data are compatible with effect sizes between the lower and upper bounds at the 95% confidence level.
Role of the Funding Source: The National Institute on Drug Abuse had no role in the study design, conduct, or analysis.
RESULTS
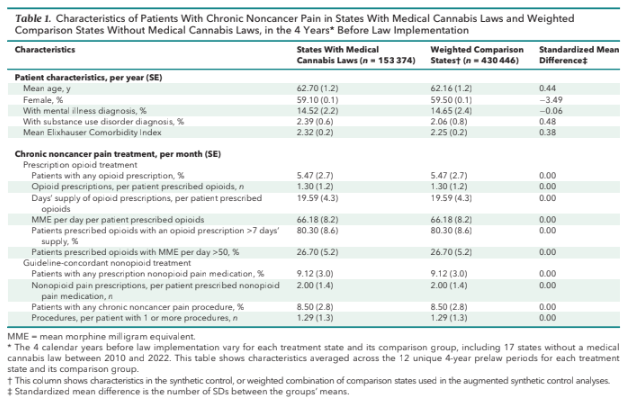
Table 1 shows the balance in prelaw patient characteristics in medical cannabis law states and synthetic controls in the augmented synthetic control approach including age (62.70 years in cannabis law states and 62.16years in synthetic controls); the proportion of females (59.10%
and 59.50%), with a mental illness diagnosis (14.52% and14.65%), and with a substance use disorder diagnosis(2.39% and 2.06%); and mean Elixhauser ComorbidityIndex (2.32 and 2.25). Medical cannabis law states and their synthetic controls had identical mean outcomes over the
4-year period before law implementation. The unweighted and state-specific comparisons are shown in Section B of the Supplement (available at Annals.org).In a given month during the 4 years before law implementation in medical cannabis law states and their syn-
thetic controls, an estimated average of 5.47% of patients received any opioid prescription, 9.12% received any nonopioid prescription pain medication, and 8.50% received any pain procedure. In a given month during the first 3 years after law implementation, medical cannabis law
states had an average decrease of 1.07 percentage points in the proportion of patients receiving any opioid prescription, relative to a 1.12 percentage point decrease in the synthetic control group; an average increase of 1.14 percentage points in the proportion of patients receiving
any nonopioid prescription pain medication, relative to a 1.19 percentage point increase in the synthetic control group; and a 0.17 percentage point decrease in the proportion of patients receiving any pain procedure, relative to a 0.001 percentage point decrease in the synthetic
control group. This translates to average differences of 0.05 percentage points (95% CI, 0.12 to 0.21 percentage points), 0.05 percentage points (CI, 0.13 to 0.23 percentage points), and 0.17 percentage points (CI, 0.42 to 0.08 percentage points) in the proportion of
patients receiving any opioid prescription, any nonopioid prescription pain medication, or any chronic pain procedure attributable to state medical cannabis laws, respectively (Figure 1).
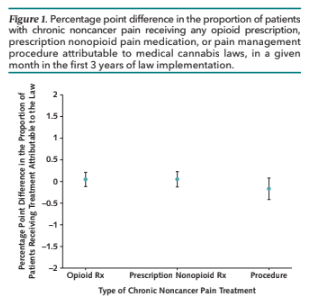
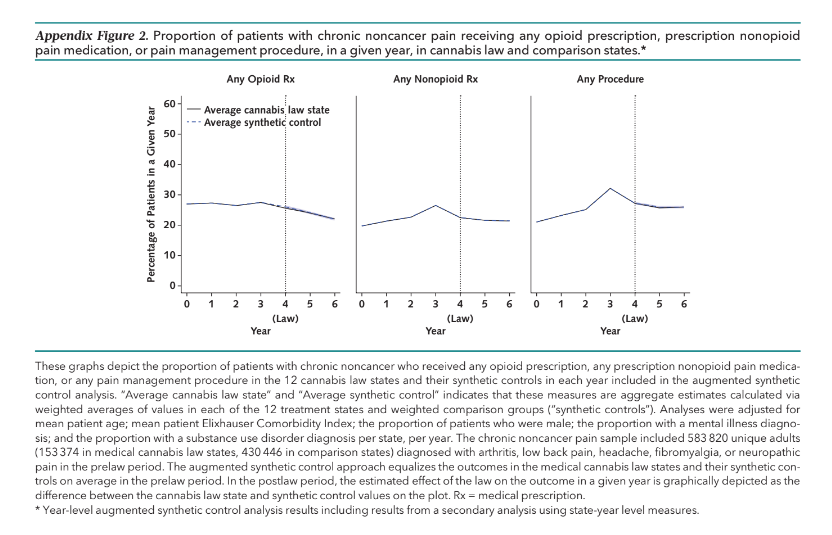
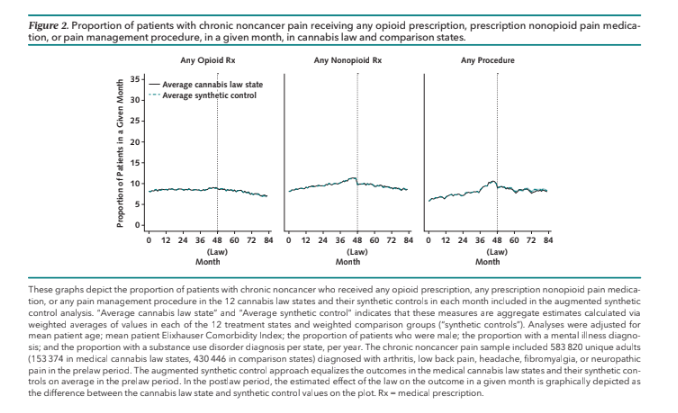
Figure 2 shows identical magnitude in the proportion of patients receiving any opioid prescription, nonopioid prescription pain medication, or a pain procedure in medical cannabis law states and their synthetic controls in each month during the 4 years before law implementation, as
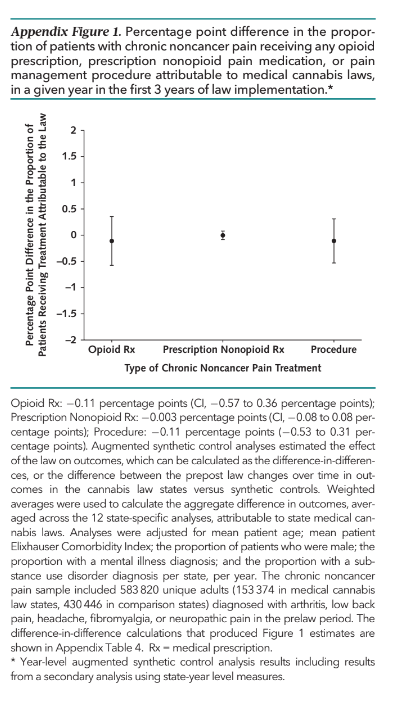
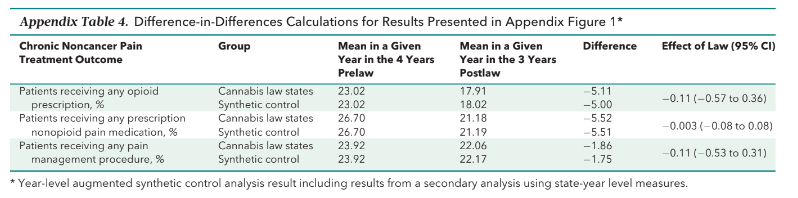
expected in the augmented synthetic control approach, and similar magnitude of these outcomes in medical cannabis law states and their synthetic controls in each month in the 3-year post-law period (Figure 2). In year-level augmented synthetic control analyses, state medical cannabis laws led to average decreases of 0.11 percentage points (CI, 0.57 to 0.36 percentage points), 0.003 percentage points (CI, 0.08 to 0.08 percentage points), and 0.11 percentage points (CI, 0.53 to 0.31 percentage points) in the proportion of patients receiving any opioid prescription, prescription nonopioid pain medication, or procedure in a given year during the post-law period, respectively, relative to predicted out-comes in the absence of the law. These results are shown graphically in Appendix Figure 1 (available at Annals.org).
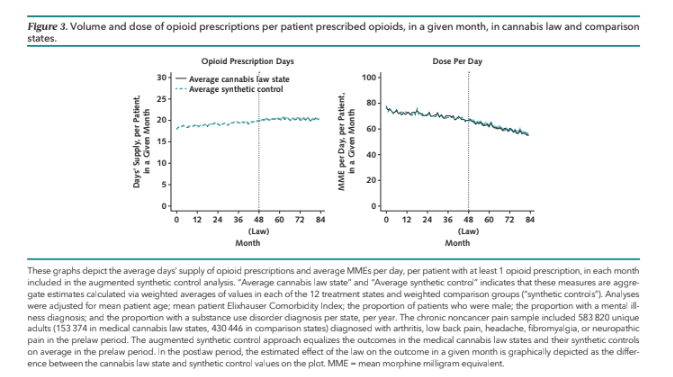
The difference-in-differences calculations that produced these estimates are shown in Appendix Table 4 (available at Annals.org). Augmented synthetic control analyses showed a similar magnitude of these outcomes in medical cannabis law states and synthetic controls in each of the 3 post-law years (Appendix Figure 2, available at Annals.org). In a given month during the first 3 years of implementation, state medical cannabis laws led to average decreases of 0.10 days’ supply (CI, 0.31 to 0.12 days’ supply) and 0.48 MMEs per day (CI, 1.86 to 0.90
MMEs per day) per patient prescribed opioids; a decrease of 1.1 percentage points (CI, 1.96 to 0.25 percentage points) in the proportion of patients receiving a prescription with greater than 7 days’ supply; and an increase of 0.31 percentage points (CI, 0.41 to 1.02 percentage
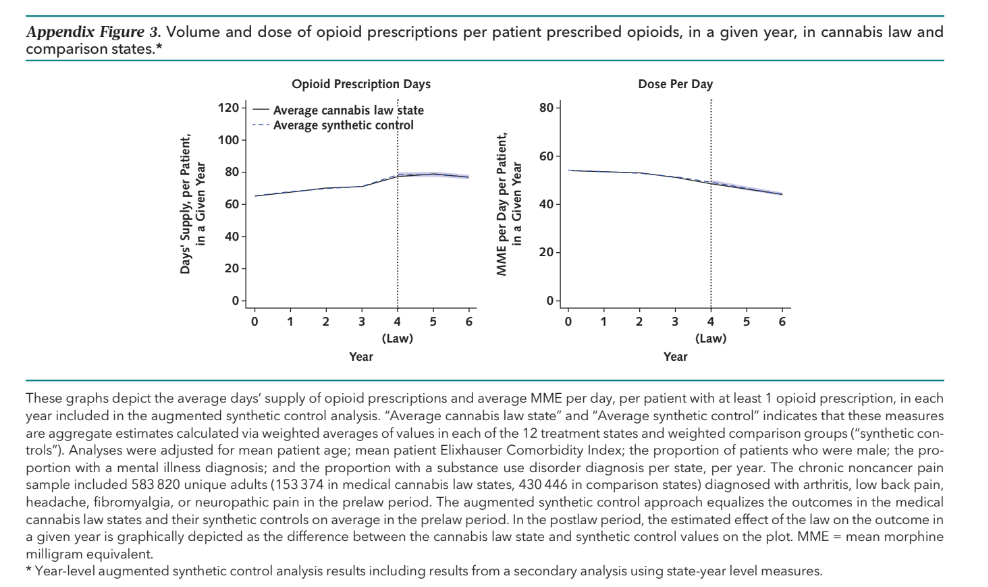
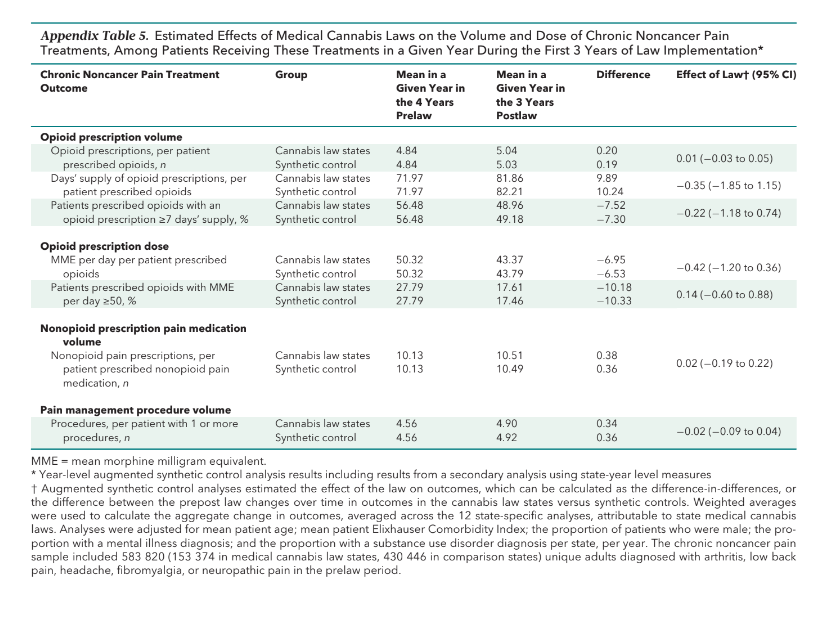
points) in the proportion of patients prescribed opioids with greater than 50 MMEs per day, relative to predicted outcomes in the absence of the law (Table 2). Augmented synthetic control analyses showed similar days’ supply and MMEs per day of opioid prescriptions in medical cannabis law states and their synthetic controls in each month of the 3-year post-law period (Figure 3). In a given year during the first 3 years of law implementation, state medical cannabis laws led to an average decrease of 0.35 days’ supply (CI, 1.85 to 1.15 days
supply) of opioid prescriptions; an average decrease of 0.42 MMEs per day (CI, 1.20 to 0.36 MMEs per day); an average decrease of 0.22 percentage points (CI, 1.18 to 0.74 percentage points) in the proportion of patients prescribed opioids with greater than 7 days’ sup-
ply; and an average increase of 0.14 percentage points (CI, 0.60 to 0.88 percentage points) in the proportion of patients prescribed opioids with greater than 50 MMEs per day. In each of the 3 post-law years, augmented synthetic control analyses showed a similar magnitude of these outcomes in medical cannabis law states and synthetic controls (Appendix Figure 3 and Appendix Table 5, available at Annals.org). The effects of medical cannabis laws aggregated across the 12 treatment states were consistent with the state-specific effect estimates averaged over the 3-year post-law period (Section C of the Supplement, available at Annals.org) and month by month (Section D of the Supplement, available at Annals.org). Although there were a few isolated statistically significant differences in outcomes attributable to state medical cannabis laws in these analyses, no clear patterns emerged. Results of sensitivity analyses accounting for state opioid-prescribing
laws were consistent with the main results (Section E of the Supplement, available at Annals.org). Annotated code for all analyses is in Section F of the Supplement (available at Annals.org).
DISCUSSION: The small-in-magnitude effect estimates and narrow confidence bounds rule out an important effect of medical cannabis laws on the chronic noncancer pain treatment outcomes measured, in either direction. Medical cannabis laws had an average estimated effect of less than 0.2 percentage points on the proportion of patients receiving any opioid prescription, nonopioid pain medication prescription, or pain procedure in a given month during the first 3 years of law implementation, with confidence intervals not exceeding a 0.5 percentage point increase or decrease. Laws’ estimated effects on these outcomes over the course of a given year during the first 3 years of implementation were similarly small in magnitude, with confidence intervals not exceeding a 0.6 percentage point increase or decrease in the proportion of patients with chronic noncancer pain receiving opioid or nonopioid treatments. Among patients prescribed opioids, the average estimated effects of medical cannabis laws on days’ supply and dose were consistently small in magnitude. Confidence intervals across monthly and yearly effect estimates did not exceed an increase or decrease of 2 days’ supply, 2 MMEs per day, or 2 percentage points in the
proportion of patients receiving an opioid prescription with greater than 7 days’ supply or 50 MMEs per day attributable to medical cannabis laws. A recent survey of a representative sample of adults with chronic noncancer pain in states with medical cannabis laws found that 31% had used cannabis to manage their pain, and that over half of adults who had used cannabis for chronic noncancer pain management perceived that the use of cannabis led them to decrease the use of prescription opioid and nonopioid pain medications (34). Our results suggest that such substitution has not led to large shifts in pain treatment patterns at the population level. Our findings are consistent with prospective research showing that cannabis use by people with chronic pain was not associated with reduced use of prescribed opioids (24). Slow implementation could contribute to study findings, as key implementation processes in many states, such as physician certification to recommend cannabis, rolled out gradually (35–37). Study results did not suggest this type of ramp-up effect, but we only examined the first
3 years of medical cannabis law implementation. Results may also be explained by reluctance, among health system leaders and individual clinicians, to recommend can-nabis for chronic noncancer pain in the face of continued federal Schedule I classification of cannabis; limited and mixed evidence on safety and effectiveness; absence of clinical guidelines; and lack of medical education on managing chronic noncancer pain with cannabis (38). As prior studies suggest an association between medical cannabis laws and reduced opioid prescribing

used general population samples including but not limited to people with chronic noncancer pain (14–21), it is possible their results were driven by state laws limiting opioid prescribing for acute pain, some of which were enacted at or around the same time as medical cannabis
laws. State opioid-prescribing limit laws have reduced opioid prescribing for acute pain (39–42) but had no effects on opioid-prescribing patterns for chronic non-cancer pain (43, 44). The single prior study examining the association between medical cannabis laws and receipt of prescription opioids among adults with chronic non-cancer pain found small but statistically significant reductions attributable to medical cannabis laws from 2006 to 2014 (21), a period encompassing upward secular trends in opioid prescribing until 2011 when opioid prescribing
volume peaked (45). It is possible that medical cannabis laws led to the greater substitution of cannabis in place of prescribed opioids during this period. Since 2011, opioid prescriptions have declined by 40% in the United States overall and by 51% among the commercially insured
(45). Our findings suggest that these downward trends are more likely driven by evolving medical norms, clinical guidelines’ increased emphasis on nonopioid approaches, and patient and physician preferences for nonopioid treatments (11, 46, 47) than by medical cannabis laws. This study has limitations. This study used a strong nonexperimental design, but causal inference does rely on untestable assumptions involving parallel counterfactual trends (31). Statistical power is limited by the constrained number of states, though the consistently small-in-magni- tude effect estimates and narrow confidence bounds lessen concern about lack of power. This study’s commercially insured sample may not generalize to other groups, though most people who use medical cannabis have commercial insurance (48, 49). Analyses did not include over-the-counter pain medications, which are not covered by insurance, or account for changes in the volume of medical cannabis dispensaries over time. Because cannabis is not covered by insurance, we could not observe patient-level substitution of cannabis in place of prescription opioids in the insurance claims data, though some substitution—for example, a clinician recommending cannabis for a new-onset chronic noncancer pain issue, when before law enactment she would have recommended prescription opioids—is inherently unobservable. Our analysis could be subject to unmeasured confounding from health system initiatives to reduce high-risk opioid prescribing and/or increasing the use of guideline-concordant nonopioid pain treatments, though these initiatives would have to differ systematically over time across treatment and comparison states (50). Our analysis did not assess cannabis laws’ effects on the clinical appropriateness of pain treatment or patient-reported pain management. The relationship between medical cannabis laws and opioid overdose was outside of the scope of this study and should be considered in future work. In conclusion, this study did not identify the important effects of medical cannabis laws on the receipt of opioid or nonopioid pain treatment among patients with chronic noncancer pain. From Division of Health Policy and Economics, Weill Cornell Medicine, New York, New York (E.E.M.); Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland (K.N.T., N.J.S., A.D.M., L.R., S.A.W.); Departments of Anesthesiology and Health Management and Policy, School of Public Health, University of Michigan, Ann Arbor, Michigan (M.C.B.); and Department of Mental Health,
Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland (E.A.S.).
Grant Support: By National Institutes of Health National Institute
on Drug Abuse grant R01DA049789.
Disclosures: Disclosures can be viewed at www.acponline.org/
authors/icmje/ConflictOfInterestForms.do?msNum=M23-0053.
Reproducible Research Statement: Study protocol: See McGinty et al (25). Statistical code: See Section F of the Supplement (avail-
able at Annals.org). Data set: Not available due to the terms of the licensing agreement.
Corresponding Author: Emma E. McGinty, PhD, Division of Health
Policy and Economics, Weill Cornell Medicine, 402 E. 67th Street,
New York, NY 10065; e-mail, emm4010@med.cornell.edu.
Author contributions are available at Annals.org.
References:
- Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic
pain among adults in the United States. Pain. 2022;163:e328-e332.
[PMID: 33990113] doi:10.1097/j.pain.0000000000002291 - National Conference of State Legislatures. State Cannabis Policy
Enactment Database. Accessed at www.ncsl.org/research/health/
state-cannabis-policy-enactment-database.aspx on 7 June 2023. - Centers for Disease Control and Prevention National Center for
Health Statistics. U.S. Overdose Deaths in 2021 Increased Half as
Much as in 2020 – But Are Still Up 15%. 11 May 2022. Accessed at
www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.
htm on 3 January 2023. - National Cannabis Industry Association. Combating the Opioid
Epidemic. October 2016. Accessed at https://thecannabisindustry.
org/combating-the-opioid-epidemic on 27 November 2022. - Lange K. Why some people think medical marijuana is a key to ending the opioid epidemic. 17 November 2017. Accessed at www.indystar.com/story/news/politics/2017/11/17/why-some-people-think-medical-marijuana-is the-key-ending-opioid-epidemic-marijuana-advocates-think-s/873816001 on 27 November 2022.
- Voelker R. States move to substitute opioids with medical marijuana to quell the epidemic. JAMA. 2018;320:2408-2410. [PMID: 30484825]doi:10.1001/jama.2018.17329
- Humphreys K, Saitz R. Should physicians recommend replacing
opioids with cannabis? JAMA. 2019;321:639-640. [PMID: 30707218]
doi:10.1001/jama.2019.0077 - Frieden TR, Houry D. Reducing the risks of relief–the CDC
opioid-prescribing guideline. N Engl J Med. 2016;374:1501-1504.
[PMID: 26977701] doi:10.1056/NEJMp1515917 - Renthal W. Seeking balance between pain relief and safety: CDC
issues new opioid-prescribing guidelines. JAMA Neurol. 2016;73:513-PMID: 26978030] doi:10.1001/jamaneurol.2016.0535 - Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing
opioids for chronic pain–United States, 2016. JAMA. 2016;315:1624-[PMID: 6977696] doi:10.1001/jama.2016.1464 - Dowell D, Ragan KR, Jones CM, et al. CDC clinical practice guide-
line for prescribing opioids for pain – United States, 2022. MMWRRecomm Rep. 2022;71:1-95. [PMID: 36327391] doi:10.15585/mmwr.rr7103a1 - National Academies of Sciences, Engineering, and Medicine.
The Health Effects of Cannabis and Cannabinoids. The Current
State of Evidence and Recommendations for Research. National
Academies Pr; 2017. - Mücke M, Phillips T, Radbruch L, et al. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane database Syst Rev. 2018;3:CD012182. [PMID: 29513392] oi:10.1002/14651858.CD012182.pub2
- McMichael BJ, Van Horn RL, Viscusi WK. The impact of cannabis
access laws on opioid prescribing. J Health Econ. 2020;69:102273.
[PMID: 31865260] doi:10.1016/j.jhealeco.2019.102273 - Bradford AC, Bradford WD. Medical marijuana laws may be
associated with a decline in the number of prescriptions for
Medicaid enrollees. Health Aff (Millwood). 2017;36:945-951.
[PMID: 28424215] doi:10.1377/hlthaff.2016.1135 - Bradford AC, Bradford WD. Medical marijuana laws reduce
prescription medication use in Medicare Part D. Health Aff
(Millwood). 2016;35:1230-1236. [PMID: 27385238] doi:10.1377/
hlthaff.2015.1661 - Liang D, Bao Y, Wallace M, et al. Medical cannabis legalization and opioid prescriptions: evidence on US Medicaid enrollees during 1993-2014. Addiction. 2018;113:2060-2070. [PMID: 29989239]
- Wen H, Hockenberry JM. Association of medical and adult-us Marijuana laws with opioid prescribing for Medicaid enrollees.
JAMA Intern Med. 2018;178:673-679. [PMID: 29610827] doi:10.1001/
jamainternmed.2018.1007 - Bradford AC, Bradford WD, Abraham A, et al. Association
between US state medical cannabis laws and opioid prescribing in
the Medicare Part D population. JAMA Intern Med. 2018;178:667-PMID: 29610897] doi:10.1001/jamainternmed.2018.0266 - Lopez CD, Boddapati V, Jobin CM, et al. State medical canna-
bis laws associated with reduction in opioid prescriptions by ortho paedic surgeons in Medicare Part D cohort. J Am Acad OrthopSurg. 2021;29:e188-e197. [PMID: 32404683] doi:10.5435/JAAOS-D-19-00767 - Shah A, Hayes CJ, Lakkad M, et al. Impact of medical marijuana legalization on opioid use, chronic opioid use, and high-risk opioid use. J Gen Intern Med. 2019;34:1419-1426. [PMID: 30684198]doi:10.1007/s11606-018-4782-2
- Caputi TL, Humphreys K. Medical marijuana users are more likely to use prescription drugs medically and nonmedically. J Addict Med. 2018;12:295-299. [PMID: 29664895] doi:10.1097/ADM.0000000000000405
- Gorfinkel LR, Stohl M, Greenstein E, et al. Is cannabis being used as a substitute for non-medical opioids by adults with problem substance use in the United States? A within-person analysis. Addiction. 2021;116:1113-1121. [PMID: 33029914] doi:10.1111/add.15228
- Campbell G, Hall WD, Peacock A, et al. Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings
from a 4-year prospective cohort study. Lancet Public Health. 2018;3: e341-e350. [PMID: 29976328] doi:10.1016/S2468-2667(18)30110-5 - McGinty EE, Tormohlen KN, Barry CL, et al. Protocol: a mixed-methods study of how the implementation of US state medical cannabis laws affects treatment of chronic non-cancer pain and adverse opioid outcomes. Implement Sci. 2021;16:2. [PMID: 33413454] doi:10.1186/ s13012-020-01071-2
- Wagenaar AC, Burris S, eds. Public Health Law Research: Theory and Methods. Jossey-Bass; 2013.
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. National Academies Pr; 2011.
- Pacula RL, Powell D, Heaton P, et al. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J
Policy Anal Manage. 2015;34:7-31. [PMID: 25558490] doi:10.1002/pam.21804
- Freisthler B, Gruenewald PJ, Wolf JP. Examining the relationship between marijuana use, medical marijuana dispensaries, and abusive and neglectful parenting. Child Abuse Negl. 2015;48:170-PMID: 26198452] doi:10.1016/j.chiabu.2015.07.008
- Shih RA, Rodriguez A, Parast L, et al. Associations between young adult marijuana outcomes and availability of medical marijuana dispensaries and storefront signage. Addiction. 2019;114:2162-2170. [PMID:31183908] doi:10.1111/add.14711
- Ben-Michael E, Feller A, Rothstein J. The augmented synthetic control method. J Am Stat Assoc. 2021;116:1789-1803.
- Hartung J, Knapp G, Sinha BK. Statistical Meta-Analysis With Applications. Wiley; 2008:36.
- Davis CS, Liberman AJ. Laws limiting prescribing and dispensing of
opioids in the United States, 1989-2019. Addiction. 2021;116:1817-[PMID: 33245795] doi:10.1111/add.15359 - Bicket MC, Stone EM, McGinty EE. Use of cannabis and other
pain treatments among adults with chronic pain in US states with
medical cannabis programs. JAMA Netw Open. 2023;6:e2249797.
[PMID: 36607641] doi:10.1001/jamanetworkopen.2022.49797 - Lamonica AK, Boeri M, Anderson T. Gaps in medical marijuana policy implementation: Real-time perspectives from marijuana dispensary entrepreneurs, health care professionals, and medical marijuana patients. Drugs: Education, Prevention, and Policy. 2016;23:422-434.
- Ruheel MA, Gomes Z, Usman S, et al. Facilitators and barriers to the regulation of medical cannabis: a scoping review of the peer-reviewed literature. Harm Reduct J. 2021;18:106. [PMID: 34649577]doi:10.1186/s12954-021-00547-8
- Boehnke KF, Dean O, Haffajee RL, et al. U.S. trends in registration for medical cannabis and reasons for use from 2016 to 2020:an observational study. Ann Intern Med. 2022;175:945-951. [PMID: 35696691] doi:10.7326/M22-0217
- Cheng KYC, Harnett JE, Davis SR, et al. Healthcare professionals’ perspectives on the use of medicinal cannabis to manage chronic pain: a systematic search and narrative review. Pain Pract. 2022;22:718-732. [PMID: 36055965] doi:10.1111/papr.13161
- Reid DBC, Shah KN, Shapiro BH, et al. Opioid-limiting legislationassociated with reduced postoperative prescribing after surgery for
traumatic orthopaedic injuries. J Orthop Trauma. 2020;34:e114-e120. [PMID: 31688409] doi:10.1097/BOT.0000000000001673 - Schmid I, Stuart EA, McCourt AD, et al. Effects of state opioid pre-
scribing cap laws on opioid prescribing after surgery. Health Serv Res.022;57:1154-1164. [PMID: 35801988] doi:10.1111/1475-6773.14023 - Reid DBC, Shah KN, Ruddell JH, et al. Effect of narcotic prescription limiting legislation on opioid utilization following lumbar spine surgery. Spine J. 2019;19:717-725. [PMID: 30223089] doi:10.1016/j.spinee.2018.09.007
- Potnuru P, Dudaryk R, Gebhard RE, et al. Opioid prescriptions for acute pain after outpatient surgery at a large public university-affiliated
hospital: impact of state legislation in Florida. Surgery. 2019;166:375-[PMID: 31196705] doi:10.1016/j.surg.2019.04.022 - McGinty EE, Bicket MC, Seewald NJ, et al. Effects of state opioid prescribing laws on use of opioid and other pain treatments
among commercially insured U.S. adults. Ann Intern Med.2022;175:617-627. [PMID: 35286141] doi:10.7326/M21-4363 - McCourt AD, Tormohlen KN, Schmid I, et al. Effects of opioid
prescribing cap laws on opioid and other pain treatments among
persons with chronic pain. J Gen Intern Med. 2023;38:929-937.
[PMID: 36138276] doi:10.1007/s11606-022-07796-8. - IQVIA Institute for Human Data Science. Prescription Opioid Trends in the United States. Measuring and Understanding Progress
in the Opioid Crisis. 16 December 2020. Accessed at www.iqvia. com/insights/the-iqvia-institute/reports/prescription-opioid-trends- in-the-united-states on 27 November 2022. - Turk D, Boeri M, Abraham L, et al. Patient preferences for
osteoarthritis pain and chronic low back pain treatments in the
United States: a discrete-choice experiment. Osteoarthritis Cartilage.
2020;28:1202-1213. [PMID: 32652238] doi:10.1016/j.joca.2020.06.006 - Comerci G Jr, Katzman J, Duhigg D. Controlling the swing of
the opioid pendulum. N Engl J Med. 2018;378:691-693. [PMID:
29466151] doi:10.1056/NEJMp1713159 - Matson TE, Carrell DS, Bobb JF, et al. Prevalence of medical cannabis use and associated health conditions documented in electronic health records among primary care patients in Washington state. JAMA Netw Open. 2021;4:e219375. [PMID: 33956129] oi:10.1001/jamanetworkopen.2021.9375
- Lapham GT, Matson TE, Carrell DS, et al. Comparison of medical cannabis use reported on a confidential survey vs documented in the electronic health record among primary care patients. JAMA Netw Open. 2022;5:e2211677. [PMID: 35604691] doi:10.1001/ jamanetworkopen.2022.11677
- Zeldow B, Hatfield LA. Confounding and regression adjustment in difference-in-differences studies. Health Serv Res. 2021;56:932-[PMID: 33978956] doi:10.1111/1475-6773.13666
Author Contributions: Conception and design: E.E. McGinty,
N.J. Seewald, M.C. Bicket, A.D. McCourt, L. Rutkow, E.A. Stuart.
Analysis and interpretation of the data: E.E. McGinty, K.N. Tormohlen,
M.C. Bicket, S.A. White, E.A. Stuart.
Drafting of the article: E.E. McGinty, N.J. Seewald, A.D. McCourt,
S.A. White.
Critical revision of the article for important intellectual content:
K.N. Tormohlen, N.J. Seewald, M.C. Bicket, L. Rutkow, S.A. White,
E.A. Stuart.
Final approval of the article: E.E. McGinty, K.N. Tormohlen,
N.J. Seewald, M.C. Bicket, A.D. McCourt, L. Rutkow, S.A. White,E.A. Stuart.
Statistical expertise: N.J. Seewald, E.A. Stuart.
Obtaining of funding: E.E. McGinty, M.C. Bicket, E.A. Stuart.
Administrative, technical, or logistic support: E.E. McGinty,M.C. Bicket, S.A. White. Collection and assembly of data: E.E. McGinty, N.J. Seewald,
A.D. McCourt, S.A. White.