Early-onset cannabis use is common (eg, 12% of 14- to 15-year-olds in the US report lifetime use) and is associated with increased risk for cannabis use disorder, other psychiatric disorders, and other problems (eg, early school drop-out) during childhood and adulthood.1,2 Prospective risk factors of early-onset cannabis use remain poorly understood.
Methods | Participants provided assent and caregivers provided written informed consent to protocols approved by in-
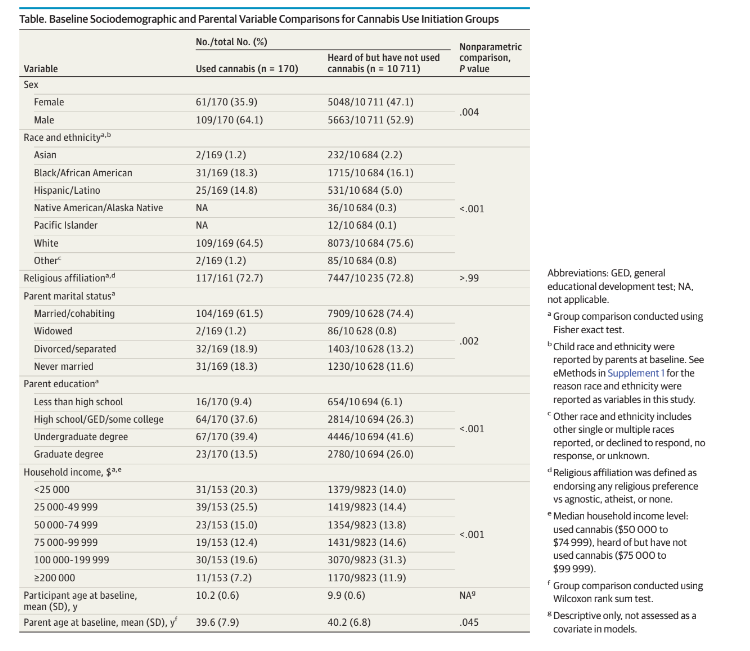
institutional review boards at each data collection site. We followed the (STROBE) reporting guideline for cohort studies. Associations between early-onset cannabis use (n = 170 [1.56 %]), defined as an endorsement of cannabis use beyond a puff in any form (ie, smoking cannabis, consuming edibles, and using concentrates, oils, or tinctures) reported at any assessment (baseline [June 1, 2016, to October 15, 2018] to 3.5-year
follow-up sessions) and psychopathology, personality, and cognition, as well as cannabis-related familial, environmental,
nesting data by collection site (lme4 package in R version 4.2.1 [R Foundation]). The no-cannabis-use group was defined as
those who had heard of cannabis by the 2-year follow-up (mean [SD] age, 12.00 [0.66] years), but not used by 3.5-year follow-up
(n = 10 711). Fixed-effect covariates included family and twin status as well as sociodemographic and parental variables
significantly associated with cannabis use (Table and Figure caption).
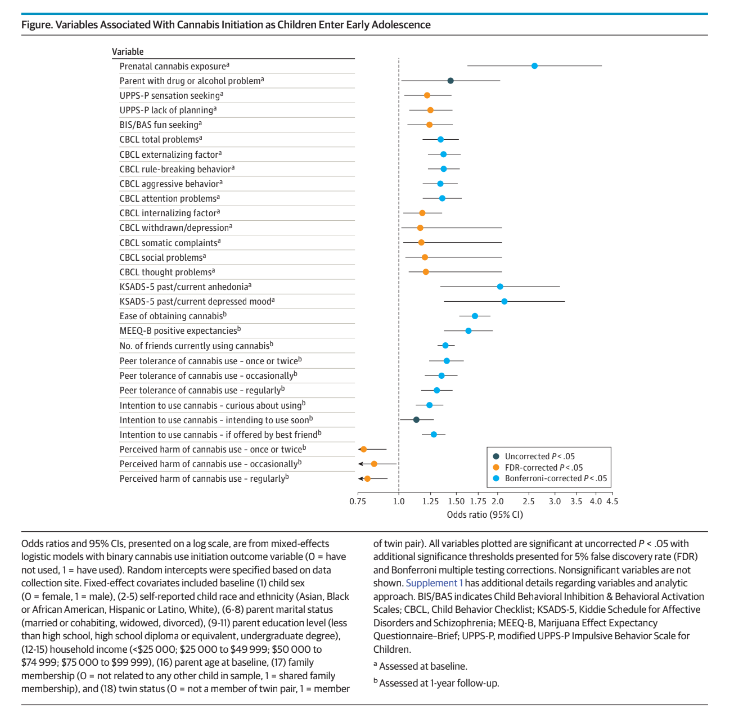
Results |Following false discovery rate correction, 29 of 46 vari-
ables were significantly associated with cannabis use initiation (Figure), 18 of which survived Bonferroni correction. As expected, initiation of alcohol and tobacco use by 3.5-year follow-up exhibited the greatest effect sizes (odds ratio [OR], 17.46;95% CI, 11.10-27.47 and OR, 35.85; 95% CI, 23.21-55.37, respectively). Outside of these associations, prenatal cannabis exposure was associated with the largest risk for cannabis use initiation (OR, 2.60; 95% CI, 1.62-4.17); this association remained when additionally controlling for alcohol and tobacco use initiation, family or parent alcohol or drug problems, and prenatal alcohol and tobacco exposure (OR, 2.16; 95% CI, 1.17-3.97). Several cannabis-specific factors at 1-year follow-up (mean [SD] age, 10.92 [0.64] years), including ease of obtaining, positive expectancies, number of friends using, and greater peer tolerance, were associated with greater odds of early initiation of cannabis use. Greater externalizing symptoms (Figure), 18 of which survived Bonferroni correction. As expected, initiation of alcohol and tobacco use by 3.5-year follow-up exhibited the greatest effect sizes (odds ratio [OR], 17.46;95% CI, 11.10-27.47 and OR, 35.85; 95% CI, 23.21-55.37, respectively). Outside of these associations, prenatal cannabis exposure was associated with the largest risk for cannabis use initiation (OR, 2.60; 95% CI, 1.62-4.17); this association remained when additionally controlling for alcohol and tobacco use initiation, family or parent alcohol or drug problems, and prenatal alcohol and tobacco exposure (OR, 2.16; 95% CI, 1.17-3.97). Several cannabis-specific factors at 1-year follow-up (mean [SD] age, 10.92 [0.64] years), including ease of obtaining, positive expectancies, number of friends using, and greater peer tolerance, were associated with greater odds of early initiation of cannabis use. Greater externalizing symptomatology, depressed mood, and anhedonia at baseline were also significantly prospectively associated with cannabis use initiation (Figure).
Discussion | Prevalence of cannabis use initiation by early adolescence in the ABCD study (1.56%) closely parallels rates of cannabis initiation observed in nationally representative samples (eg, 1.87%1 ). Prenatal cannabis exposure was associated with a more than 2-fold increase in early onset of cannabis use, independent of prenatal exposure to or use of other substances or family history of drug or alcohol problems.
Similar associations have been noted in later adolescence or adulthood,4 but our study suggests an association with early-onset use. In addition to replicating associations between externalizing behavior and early cannabis use,5 anhedonia and depressed mood at age 9 to 11 years were associated with future early-onset cannabis use, highlighting internalizing symptomatology as a risk factor for early initiation. Moreover, cannabis-related individual (eg, positive expectancies), social (eg,peer use/attitudes), and environmental (eg, ease of access) fac-
tors were associated with early onset use. Permissive social milieu in childhood and adolescence may represent a tractable target for prevention and intervention efforts.6Notwithstanding limitations of the small sample of participants having used cannabis, our findings suggest greater caution in cannabis-related attitudes, access, and use during periods of vulnerability (eg, pregnancy), particularly for youth with other mental health liabilities.
Alex P. Miller, PhD
David A. A. Baranger, PhD
Sarah E. Paul, MA
Alexander S. Hatoum, PhD
Cynthia Rogers, MD
Ryan Bogdan, PhD
Arpana Agrawal, PhD
Author Affiliations: Department of Psychiatry, Washington University School
of Medicine, St Louis, Missouri (Miller, Rogers, Agrawal); Department of
Psychological and Brain Sciences, Washington University in St Louis, St Louis,
Missouri (Baranger, Paul, Hatoum, Bogdan).
Accepted for Publication: March 31, 2023.
Published Online: June 26, 2023. doi:10.1001/jamapediatrics.2023.1801
Corresponding Author: Alex P. Miller, PhD, Department of Psychiatry,
Washington University School of Medicine, 660 S Euclid, CB 8134, St Louis, MO
63110 (m.alex@wustl.edu).
Author Contributions: Dr Miller had full access to all of the data in the study
and takes responsibility for the integrity of the data and the accuracy of the data
analysis. Drs Bogdan and Agrawal contributed equally.
Concept and design: Miller, Hatoum, Bogdan, Agrawal.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Miller, Bogdan, Agrawal.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Miller, Baranger, Hatoum, Bogdan, Agrawal.
Obtained funding: Bogdan, Agrawal.
Administrative, technical, or material support: Paul, Bogdan, Agrawal.
Supervision: Bogdan, Agrawal.
Conflict of Interest Disclosures: None reported.
Funding/Support: Data for this study were provided by the Adolescent Brain
Cognitive Development (ABCD) study, which was funded by the National
Institutes of Health grants U01DA041022, U01DA041025, U01DA041028,
U01DA041048, U01DA041089, U01DA041093, U01DA041106, U01DA041117,
U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174,
U24DA041123, and U24DA041147 and additional federal partners (https://
abcdstudy.org/federal-partners.html). Support for this study was also derived
from National Institutes of Health grants T32DA015035 (A.P.M.), F31AA029934
(S.E.P.), K01AA030083 (A.S.H.), R01DA054750 (R.B., A.A.), U01DA055367,
R01DA046224 (C.R., R.B., A.A.).
Role of the Funder/Sponsor: Beyond listed authors, no other ABCD Study
investigator contributed to this manuscript. The funders had no role in the
design and conduct of the study; collection, management, analysis, and
interpretation of the data; preparation, review, or approval of the manuscript;
and decision to submit the manuscript for publication.
Disclaimer: This article reflects the views of the authors and may not reflect the
opinions or views of the National Institutes of Health or the Adolescent Brain
Cognitive Development (ABCD) consortium investigators.
Data Sharing Statement: See Supplement 2.
Additional Contributions: We thank Deanna Barch, PhD (Department of
Psychological and Brain Sciences, Washington University in St Louis), for
providing information regarding 2020 recreational cannabis legalization status
of data collection sites, for which compensation was not received.
Additional Information: The ABCD data repository grows and changes over
time. The ABCD data used in this report came from https://dx.doi.org/10.15154/
1523041.
Substance Abuse and Mental Health Services Administration. Key substance
use and mental health indicators in the United States: results from the 2018
National Survey on Drug Use and Health. HHS Publ No PEP19-5068 NSDUH Ser
H-54. Published May 2019:51-58. https://www.samhsa.gov/data/sites/default/
files/cbhsq-reports/NSDUHNationalFindingsReport2018/
NSDUHNationalFindingsReport2018.pdf
Connor JP, Stjepanović D, Le Foll B, Hoch E, Budney AJ, Hall WD. Cannabis
use and cannabis use disorder. Nat Rev Dis Primers. 2021;7(1):16. doi:10.1038/
s41572-021-00247-4
Lisdahl KM, Sher KJ, Conway KP, et al. Adolescent brain cognitive
development (ABCD) study: overview of substance use assessment methods.
Dev Cogn Neurosci. 2018;32:80-96. doi:10.1016/j.dcn.2018.02.007
Sonon KE, Richardson GA, Cornelius JR, Kim KH, Day NL. Prenatal marijuana exposure predicts marijuana use in young adulthood. Neurotoxicol Teratol.
2015;47:10-15. doi:10.1016/j.ntt.2014.11.003
King SM, Iacono WG, McGue M. Childhood externalizing and internalizing
psychopathology in the prediction of early substance use. Addiction. 2004;99
(12):1548-1559. doi:10.1111/j.1360-0443.2004.00893.x
Turel O. Perceived ease of access and age attenuate the association between
marijuana ad exposure and marijuana use in adolescents. Health Educ Behav.
2020;47(2):311-320. doi:10.1177/1090198119894707
